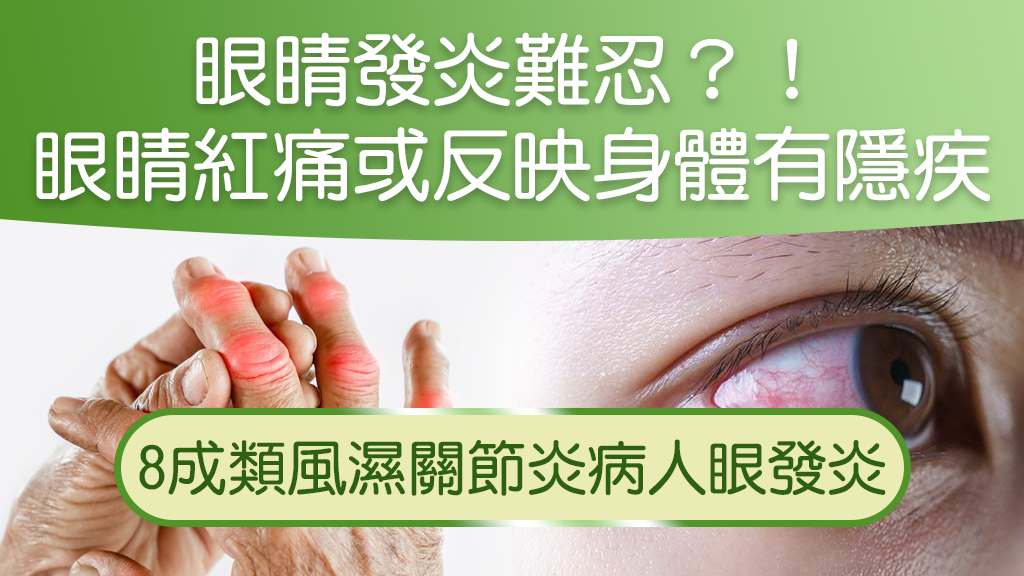
【Eye inflammation】Red and painful eyes or reflect hidden diseases in the body Doctor: 80% of rheumatoid arthritis patients have eye inflammation
Many doctors will use the eyes as a window to observe physical diseases, especially long-term patients, which diseases will affect the eyes?
Diseases that affect the eyes
Eye pain, redness, eye inflammation and other conditions, ordinary elderly people may feel, but if the situation continues, we will worry about other hidden diseases in the body, one of which is an autoimmune system disease, which will cause various inflammations in the body. The eye is also one of the affected organs, and if not looked at or treated, the eye's vision will continue to decline and there is even a risk of blindness.
Symptoms and treatment of immune system disorders
Immune system disorders occur in people of all ages, most commonly rheumatoid arthritis, xexia, ankylosing spondylitis, or lupus erythematosus. Taking rheumatoid arthritis as an example, patients may have low back pain, hip pain or inflammation, so that they have a sore back and a stalk. Calcification occurs due to inflammation. Joints will combine with each other, so that it is difficult to get up in the morning or want to bend over and reach for the toes, which will affect joint movement for a long time. First-line treatment is systemic and is usually prescribed by a rheumatoid specialist with oral anti-inflammatory drugs.
Steroids are generally used in first-line treatment, but if we use large doses of steroids, or if we continue treatment, we will generally switch to second-line drugs to reduce the side effects caused by steroids. Biologics and immunosuppressants are used as second-line agents to control long-term therapy.
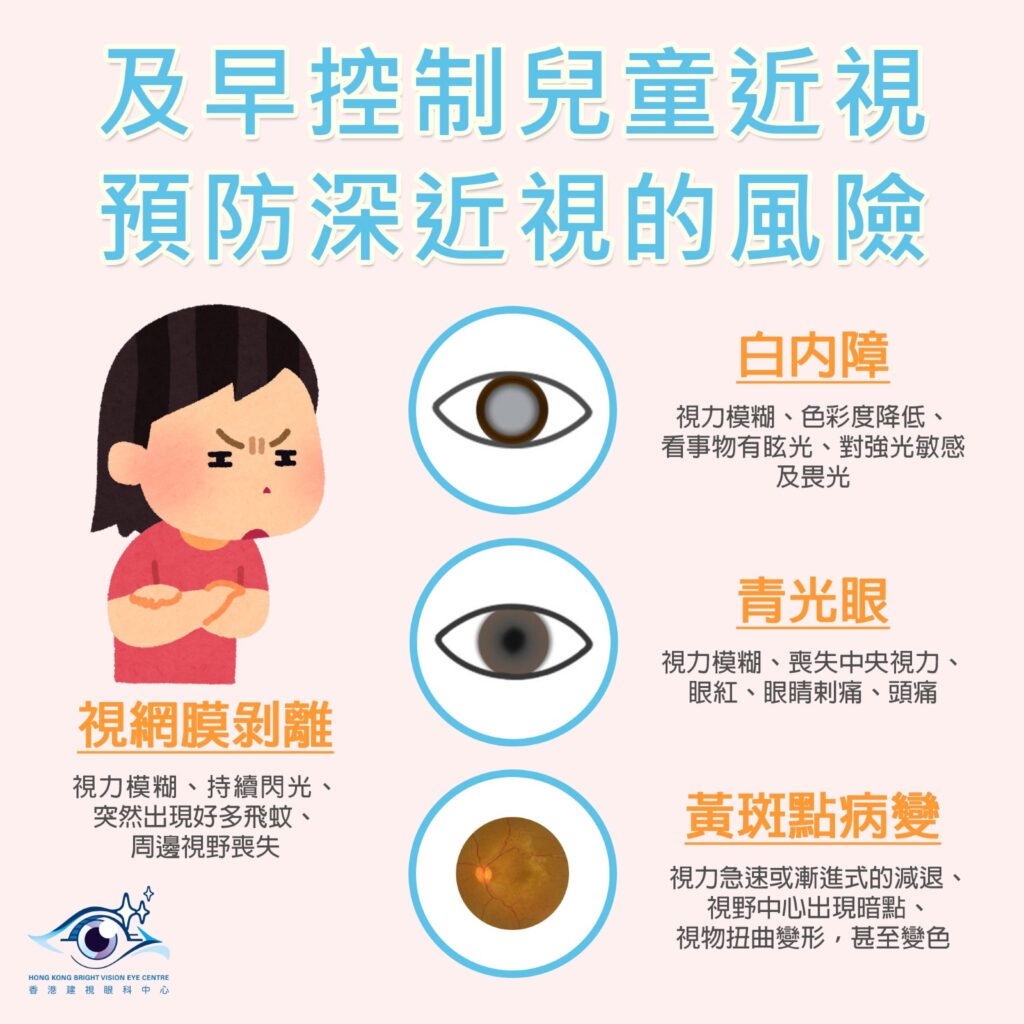
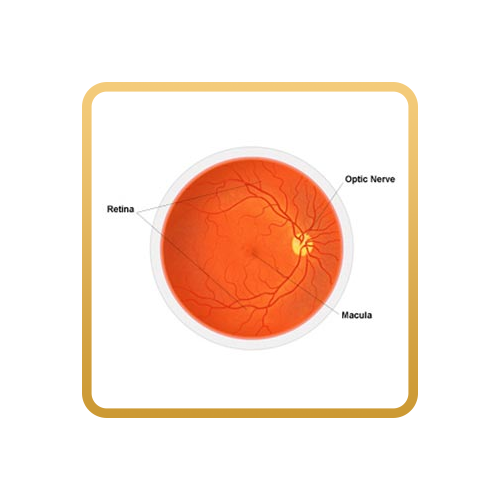
Studies have shown that eighty percent of patients have at least one chance of eye inflammation in their lifetime, iritis is one of the inflammations, it will release cells, resulting in vision loss, and these cells, will bind to the protein in the eyeball, accumulate in the anterior chamber angle, resulting in the anterior chamber angle water failure to flow away, so that intraocular pressure rises, damage nerves and form glaucoma.
TO BE TREATED, BLOOD IS USUALLY DRAWN TO FIND INFLAMMATORY FACTORS AND X-RAYS, SUCH AS LUNG X-RAYS OR LUMBAR BONE X-RAYS, TO SEE IF THERE ARE LUNG OR LUMBAR BONE PROBLEMS. IF PRESENT, A SYRUP IS USUALLY GIVEN TO CONTROL INFLAMMATION (AN ANTI-INFLAMMATORY STEROID EYE DROP). IN ADDITION, TO SEE IF THERE ARE SIDE EFFECTS AND COMPLICATIONS, USE GLAUCOMA EYE DROPS TO CONTROL INTRAOCULAR PRESSURE, SO OPHTHALMOLOGISTS AND RHEUMATOID SPECIALISTS WILL WORK TOGETHER TO CARE FOR AND TREAT PATIENTS.
lotion
There are different types of potions, some potions are ordinary moisturizing potions, which do not help the condition, and sometimes delay treatment, and some potions have the effect of constricting blood vessels, but it is not controlling inflammation, so there is a chance to mistakenly think that the eye condition continues to improve; Finally, if the treatment dose is insufficient or the medication is not used for enough time, it will delay the treatment and cause irreversible problems in the eyes.
Coronavirus
Conjunctivitis is accompanied by respiratory infections, such as influenza or viral colds, which is actually one of the symptoms of new coronary pneumonia. The most common symptom of conjunctivitis is conjunctival hyperemia or redness and inflammation of the corn of the eyeball. Studies have shown that 30 new crown patients had a test during admission and found that one of them had symptoms of conjunctivitis, so it was closely related.
To prevent the new crown pneumonia, first of all, we must wash our hands frequently, wash with water and lobe liquid for at least 20 seconds, in addition, we need to maintain a proper social distance of 1.5 meters, and we need to maintain air circulation to protect ourselves in the new crown pneumonia.
Source: Topic