Is a black spot in the eye a precursor to blindness? Ophthalmologist explains in detail the treatment and improvement of floaters
Floaters are sometimes annoying, people with floaters will see "black spots" floating in their eyes, not painful or itchy and unable to rub open, when you look directly at them, they will disappear in an instant. Floaters come in different shapes, such as black dots, lines, circles, ovals, tadpoles, etc., especially when looking at a bright and clean background, it is easier to spot its presence. Floaters are a degenerative disease of the eyes, mild patients in general, as long as they are used to coexisting with black spots and floating objects in the eyes, daily life is not affected, they do not need to receive floaters treatment, but if the black spots or floating objects in the eyes are too large or too much, floaters suddenly attack or flash, so that vision is damaged, you should seek improvement methods, find an ophthalmologist for the treatment of floaters for consultation and surgery or laser treatment of floaters, otherwise, the longer it drags on, the more serious or blind!
What is floaters?
Floaters are medically a phenomenon of vitreous degeneration of the eye. The vitreous is a transparent gel located behind the lens and before the retina. Normally, the vitreous fills the entire vitreous cavity to support the shape of the eyeball. But with age, myopia and other problems, the vitreous will liquefy and shrink, forming turbid fibers, and these fibers will float around in the vitreous, when the light refracts these fibers, the patient will feel that there are black spots in the eyes, which is the precursor of floaters.
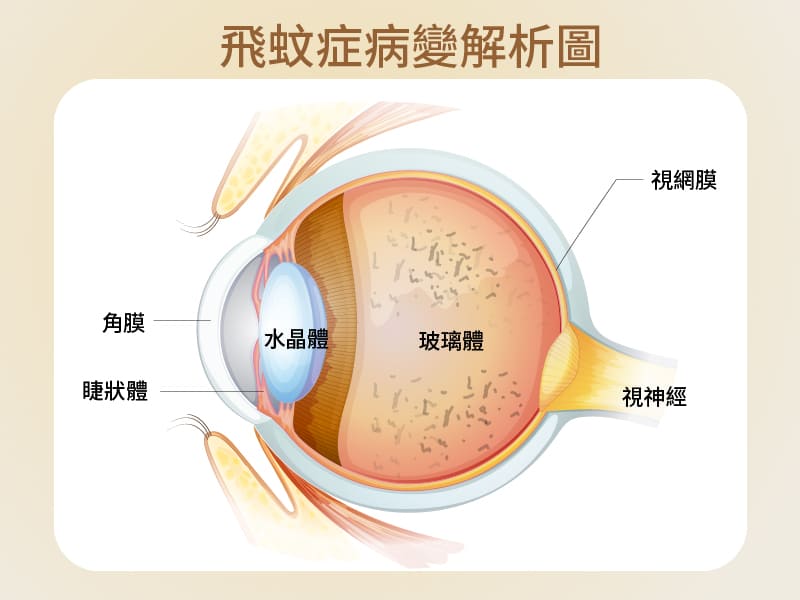
Floaters are medically a phenomenon of vitreous degeneration of the eye. The vitreous is a transparent gel located behind the lens and before the retina. Normally, the vitreous fills the entire vitreous cavity to support the shape of the eyeball. But with age, myopia and other problems, the vitreous will liquefy and shrink, forming turbid fibers, and these fibers will float around in the vitreous, when the light refracts these fibers, the patient will feel that there are black spots in the eyes, which is the precursor of floaters.
Who is most likely to develop floaters?
Floaters usually become more common with age, so older people are more likely to have dark spots in their eyes. But in addition to age, other factors that may increase the risk of floaters include myopia, history of eye surgery, eye trauma or eye inflammation. According to clinical studies, high-risk groups for floaters include:
- Middle-aged and elderly
- People with high myopia
- People with hypertension/diabetes
- Have had eye surgery
- Blows to the head, e.g. car accidents, divers
- Other eye problems, such as eye inflammation
However, most floaters are benign, such as because of old vitreous degeneration, or excessive eye fatigue, there may be symptoms of floaters, as long as there are more black spots in the eyes, and the position is fixed, do not worry too much.
Conversely, if suddenly there are a large number of dark spots in the eye that have affected the field of vision or there is a flash, it may be vitreous peeling, resulting in pulling the retina to the hole or even falling off. This condition must be investigated immediately, for improvement, or for floaters.
Causes of floaters
The causes of floaters can be broadly divided into three types, namely physiological, degenerative and pathological.
- Physiological
About 80% of floaters are physiological. Physiological floaters usually occur in people under the age of 40 or people who have been using their eyes for a long time, and most people will see black spots in the eyes, which are vitreous impurities that usually do not affect vision, and do not need to be treated immediately for floaters, and will disappear on their own over time
- Degenerative
As we age, the vitreous body of the eyeball, like other organs in the body, gradually deteriorates. In this degeneration process, the vitreous body will shrink to form fine fibers, these fibers will float in the glass, when the light enters the eye, and these impurities refract, it is the black spots in our eyes.
- Pathological
Pathological floaters are caused by eye disease or systemic vascular disease. The so-called eye disease refers to the retina under the pull or degeneration of the process of the retina in the process of tearing or degeneration, resulting in vitreous hemorrhage, and even retinal peeling, resulting in visual impairment, and in the worst case, permanent blindness. In addition, systemic vascular diseases, such as eye stroke, diabetes, hypertension or macular degeneration, if not paid attention to and actively treated, may also appear pathological floaters, patients should seek to improve floaters as soon as possible.
Complications of floaters – retinal detachment/tear

Although suffering from floaters is not a serious disease, retinal detachment caused by floaters is an emergency in ophthalmology. One in four people with floaters may have their vision affected by retinal detachment or a tear. Keep in mind that if you have these signs of retinal detachment due to floaters, including:
- There are a large number of dark spots in the eyes in a short time
- Unusual flashes
- shadow
- The view is blocked
This means that there may be cracks in the retina, and it is important to seek immediate medical attention for treatment, otherwise floaters will cause permanent damage to vision or even blindness.
How is floaters treated?
If you have benign floaters, you do not need to be treated immediately. When you notice dark spots in your eyes, you can try moving the eyes to let the fluid flow through the eyes so that the fibers leave the line of sight. Of course, some people can't bear the black spots floating around in their eyes, and their attention is often disturbed by black spots, which seriously affects their mood, so they can consider floaters treatment.
With current technology, the main treatment and improvement of floaters is laser therapy and vitrectomy.
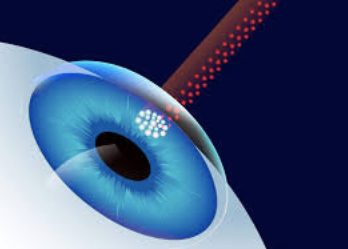
First, laser treatment of floaters
This floater treatment is suitable for large and concentrated vitreous fibers, using laser light to break these fibers into smaller fragments, through these methods to improve and eliminate floater symptoms. The laser treatment is performed under local anesthesia without pain and the whole treatment takes only 15 to 20 minutes. However, not everyone is suitable for laser treatment to improve floaters, and if the fibers are loose or too close to the macula or crystals, it should not be performed to avoid complications such as cataracts or macular damage.
Second, vitrectomy surgery to treat floaters
Vitrectomy is performed by removing the vitreous inside the eye through a small incision and replacing it with a solution to maintain the shape of the eye. The procedure only takes about 10 to 15 minutes. However, vitrectomy does not necessarily completely remove the fibers, and if the surgery itself causes bleeding or retinal tears, new floats may form, so most physicians do not recommend this procedure to treat floaters.
Floaters improvement and maintenance methods
Once floaters occur, it is almost difficult to reverse, even after laser or surgical treatment, there is a possibility of recurrence, what we can do is to live peacefully with it, or we can improve floaters by the following methods to reduce symptoms slightly.
First, the daily maintenance of benign floaters
- Avoid excessive eye use
PAY ATTENTION NOT TO OVERWORK THE EYES, ESPECIALLY 3C HEAVY USERS, YOU SHOULD LET THE EYES REST FOR 5 TO 10 MINUTES EVERY 1 HOUR, USE THE REST TIME TO BLINK, LOOK INTO THE DISTANCE TO RELAX THE EYES.
- Good living habits
In daily life, it is recommended to reduce the time spent playing with mobile phones, especially to avoid staying up late at night to look at mobile phones, to ensure that you have enough sleep and do exercise in a timely manner, which is also a way to improve floaters.
- Regular follow-up
Do not think that you have benign floaters can relax, floaters must be regularly checked to avoid other lesions, miss the best time for treatment.
- Eye care diet
Foods with antioxidant effects, such as berries, green or yellow vegetables, carrots, soybeans, milk, and fish oil, should be consumed in your diet to help improve floaters.
2. Postoperative care and maintenance of malignant floaters
- Medication treatment
After surgery, be sure to follow the doctor's instructions, remember to wash your hands thoroughly with soap before each medicine to avoid cross-infection.
- Improve your lifestyle
Rapid eye movements and excessive eye use should be avoided for 1 week after surgery. Try not to read books, mobile phones, computers, TV, etc. during this period. In addition, it is recommended not to do strenuous exercise, climbing, diving, or flying, as these activities can irritate the eyes and affect the speed of postoperative repair.
- Use an eye patch
During eye repair, it is recommended to wear an eye mask at all times to prevent collisions and avoid unconsciously rubbing your eyes when sleeping at night. It is necessary to ensure that the eye mask is clean when using, and it is recommended to wash and disinfect the eye mask daily to avoid wound infection due to bacteria.
- Daily diet
In addition to avoiding irritating foods, it is also necessary to avoid eating legumes, because such foods are easy to let the nitric oxide in the blood run into the eyes, causing the inert gas in the eyes to produce flatulence and increase the pressure in the eyes.
- Safe at home
Keep your home clean and tidy, reduce dust and avoid secondhand smoke, and do not change the layout of the home or place objects in the aisle during the recovery period, so as not to cause collisions or falls in unfamiliar environments and irritate the eyes.
- Regular follow-up visits
In addition to following the doctor's advice for regular follow-up consultations after surgery, if you notice eye discomfort, such as persistent eye pain, sudden blurred vision, nausea, increased or larger dark shadows, etc., remember to consult your ophthalmologist immediately to avoid worsening of the condition.
How can floaters be prevented?
Although we cannot completely avoid the occurrence of floaters, we can slow down the aging of the eyes and reduce the chance of developing floaters through daily maintenance.
1. Develop good eye habits
- AVOID EXCESSIVE USE OF 3C PRODUCTS (1 HOUR WITH EYES AND 5-10 MINUTES BREAK)
- Works in sufficient light and stable without flickering
- Avoid staying up late to increase the burden on your eyes
2. Intake of eye care nutrients
- Carotenoids (dark green, dark yellow and red fruits and vegetables)
- Anthocyanins (plum fruits)
- VITAMINS (VITAMINS A, B, C AND E)
- Omega3 fatty acids (fish oil)
3. Proper control of systemic vascular diseases (such as: diabetes, hypertension)
- Maintain a balanced nutrition and reduce the intake of foods high in oil and salt and sugar
- Regular exercise (jogging, cycling)
- Have regular full-body examinations
Although most floaters can not be treated, they should not be completely ignored, and they must be checked regularly, and if symptoms are aggravated, they should seek medical attention immediately to avoid missing the golden period of floater treatment.
#眼睛有黑影飄來飄去 #眼睛黑點改善 #黑眼球有黑點 #眼睛里有黑点
Is a dark spot in the eye a sign of blindness? Read More »