Age related macular degeneration

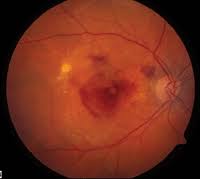
黃斑病變是一種慢性眼疾,罹患該眼疾的患者表現為中央視力模糊、扭曲、有黑點等等。眼睛黃斑點病變成因是因為位於視網膜中央的黃斑點退化或損傷,若不及時接受治療控制病情,嚴重的話有可能會導致失明。
甚麼是黃斑點?
黃斑點位於視網膜中央,主要功能是提供中間視力,這對於閱讀、駕駛和辨識面部特徵等活動至關重要。另外,黃斑點也包含大量的錐狀細胞,這些感光細胞能夠感知細節和顏色,因此是視力最敏銳的區域。由於黃斑點在視覺功能中的重要性,任何損傷或黃斑點退化(如老年黃斑病變)都會顯著影響中央視力和精細視覺能力。
黃斑部病變原因
黃斑部病變主要成因是因為一些促發因子造成氧化傷害,再加上老化傷害所形成。 隨著年齡增加,眼部的沉積物會逐漸堆積,血管也會開始增生,罹患黃斑部病變的機率也會逐漸上升。 除了年齡之外,一些不良的生活習慣也會增加眼睛罹患黃斑病變的風險。
黃斑點病變形成原因和以下因素有關:
- Age (about 10% of the incidence rate for ages 65- to 74 years; about 30% for 75-85 years of age)
- Smoking.
- Hypertension.
- Family genetics
- EXPOSURE TO PURPLE UV LIGHT FOR A LONG TIME.
- Lack of balanced nutrition.
黃斑病種類
臨床上,黃斑病變分爲兩種形態:乾性黃斑病變和濕性老年黃斑病變,其中濕性黃斑病變比乾性老年黃斑病變更嚴重,治療方法也有所不同。
乾性黃斑病變
- 乾性黃斑病變是最常見的類型,佔約8~9成。
- 成因乃視網膜細胞退化所形成的代謝物堆積所致。
- 乾性黃斑病變進展緩慢,起初可能不會對視覺造成明顯影響,但建議務必要改變不良生活習慣和多攝取護眼營養素,並且定期在家中用阿姆斯勒方格監察黃斑點的變化,如果有出現異常便需要尋求醫生進一步治療。
- 若確診乾性黃斑病變後沒有時刻監督和控制病情,視力可能會逐漸變得模糊或失去中央視覺,甚至演變成濕性老年黃斑病變。
Wet macular degeneration
- 老年黃斑病變較少見,罹患此類黃斑病變的患者有可能會失明。
- 成因是有異常的血管在黃斑區生長,導致視網膜各層受到破壞,形成視網膜出血、玻璃體出血、黃斑部水腫、視網膜結痂等。
- 老年黃斑病變進展較快,有可能在短時間內突然失明或視力嚴重下降。
- 晚期的濕性黃斑病變治療方法:眼內注射(血管內皮生長因子抑制劑)、激光光凝凝固治療、光動力療法
黃斑點病變症狀
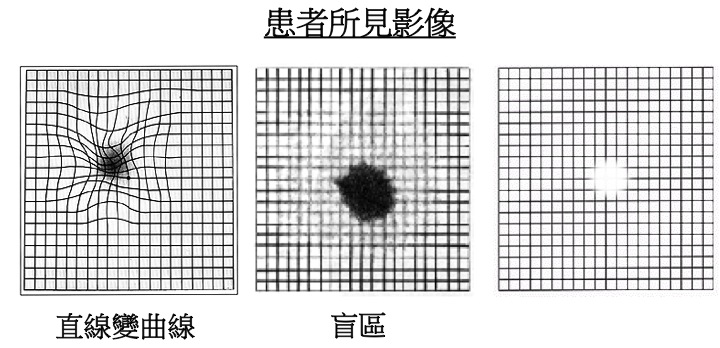
黃斑點病變症狀可能只發生在單隻眼睛,但也有可能雙眼先後出現,若是發覺中央視力有點模糊不清、影像扭曲或顔色變淺等等,基本上就可以確定是老年黃斑病變,不過還是建議到眼科診所檢查,才能做出正確判斷。
- Visual disturbances: Age-related macular degeneration affects central vision, and people feel that central vision gradually becomes blurred or has dark spots, making it difficult to recognize details, read, drive, and distinguish faces
- Altered visual field: patients may feel things deformed in the central field of view, for example, straight lines may appear curved or distorted; Distance and altitude are often misjudged
- Abnormal color vision: People with age-related macular degeneration may have problems with color perception, such as dull colors or difficulty distinguishing similar colors
黃斑點病變測試圖 - 阿姆斯勒方格表
Steps:
- Test with plenty of light and average, and place the square table at a distance of 30 cm from the line of view.
- If you have an old flower or a person with short-sightedness, you should wear the original glasses for testing.
- Cover your left eye with your hand and gaze at the black spot in the center of the square table with your right eye.
- Repeat steps 1 to 3 to check the left eye.
如果你在黃斑眼病測試過程中,發現直缐彎曲,某些地方模糊不清或缺失,或可能是老年黃斑病變的警訊,應該儘早向眼科醫生尋求建議。
黃斑病變治療方法
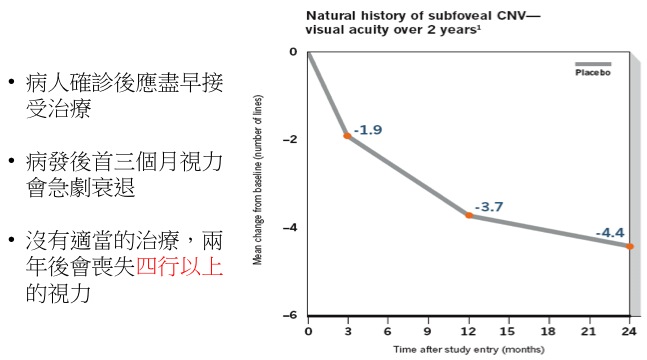
Treatment prime time.
治療方法
黃斑病變的治療取決於該疾病是處於早期乾性還是晚期的濕性。儘管營養干預可能有助於阻止其發展為濕性,但尚無 FDA 批准的乾性黃斑病治療。雖然目前尚無徹底治愈黃斑病變的方法,但某些治療方法可能會延遲其進展甚至改善視力:
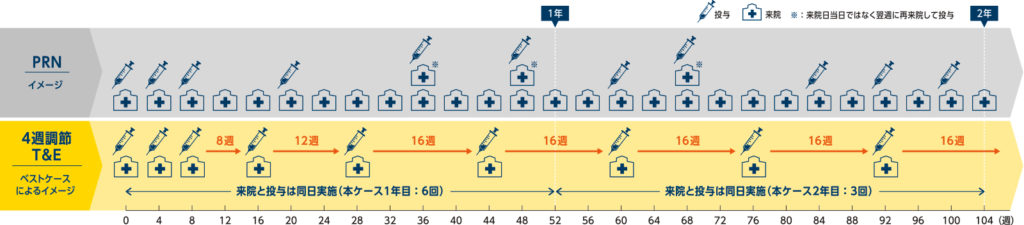
- 眼內注射血管內皮生長因子抑制劑(anti VEGF)
現今最有效的治療濕性黃斑病變方法,一般最少進行三次注射(每次相隔4星期), 繼後亦可能需要更多次的注射以穏定情況
- Laser light coagulation
激光光凝凝固是利用激光熱能去破壞異常增生的血管,阻止視力衰退。然而,這種方法可能會破壞健康的組織,因此,醫生會在術前為病患做詳細檢查再根據個案情況去推薦最好的治療方案。
- Photodynamic therapy
眼科醫生會先為患者注射感光藥水,這類藥水會依附在異常增生血管,在利用冷性激光激發感光藥水,從而破壞異常血管,進而改善視力問題。
- Low vision glasses
如果黃斑病變晚期結痂,當眼內注射藥物也沒有用時,就可以考慮配戴低視能眼鏡作為輔助的方法提升視力。
近年智慧型的低視能眼鏡十分進步,它獨特之處是,能夠即時地將週邊圖像投射到低視能人士視網膜最健康的位置上,並根據低視力人士的感知來作調整。這種眼鏡可透過補充和矯正細節,令病人對於真實場景的感知獲得改善,提高其因應性。在檢查時,眼科醫生可採用程式直觀操作來調試眼鏡,檢測低視能人士更好的視力範圍。

Standardized visual acuity chart developed by the World Health Organization (WHO) for low vision
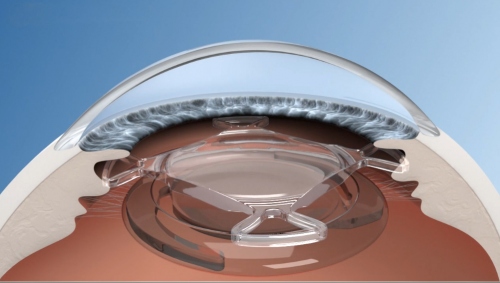
- Bifocal additional intraocular lens
SML (Scharioth Macula Lens) is a dual-focus supplementary intraocular lens developed by Professor Gabor B. Scharioth. It features a specifically designed central optical zone that provides a high additional power of +10.0D. The SML is intended for implantation in one eye to enhance near vision without compromising distance vision or visual field.

黃斑點病變食療
眼睛黃斑部病變是不可逆的,無論是進行手術還是其他治療老年黃斑病變的方案,都只能做到控制病情防止惡化。如果家中老人不幸罹患黃斑病變,則需要立即改變飲食和一些不良生活習慣,因為只有健康的身體才能有效降低黃斑部病變惡化的風險。
一些研究表明,飲食中應包含大量鮭魚和其他冷水魚,當中含有大量的 omega-3 脂肪酸,有助於預防黃斑病或降低其發展的風險。
臨床數據顯示,葉黃素和玉米黃質對於減緩黃斑點退化有一定的效果。但這類營養素並無法自行合成,需要從食物中獲取,例如玉米、蛋黃、南瓜,以及一些深綠色蔬菜如菠菜、芥蘭、地瓜葉等。在眾多蔬菜當中,羽衣甘藍的葉黃素和玉米黃質含量極高,建議平日應多吃這些蔬菜才能保護眼睛免受黃斑病侵害。
Q and A.
1. Can blackening the use of mobile phones cause macular lesions?
At present, there is not enough research data to show that the use of mobile phones and other electronic products, will directly cause macular disease, but the high-energy visible light (commonly known as blue light) emitted by smartphones, may damage the macular area. If you play with your cell phone and watch TV in a dark environment, the pupil sits in, and the macular area has the opportunity to absorb more blue light, increasing the risk of developing various eye diseases. Therefore, it is not encouraged to play with black phones.
2. Blu-ray glasses: useful or hyped?
BEFORE THE BEGINNING OF MODERN DIGITAL LIFE, WE ALREADY HAD A LOT OF BLUE LIGHT, MOSTLY FROM THE SUN. BUT GADGETS SUCH AS TVS, SMARTPHONES, LAPTOPS AND TABLETS ARE FILLED WITH MODERN LIFE, EMITTING BRIGHTER, SHORTER WAVELENGTHS (BLUER) LIGHT. THE AMERICAN ACADEMY OF OPHTHALMOLOGY (AAO) SAYS YOU DON'T NEED THEM AND DON'T RECOMMEND ANY SPECIAL GLASSES. THE GROUP SAYS BLUE LIGHT FROM SMART DEVICES DOES NOT CAUSE EYE DISEASE OR EVEN EYE FATIGUE. IT SAYS THE PROBLEM IS SIMPLY CAUSED BY THE OVERUSE OF SMART DEVICES. "THE SYMPTOMS OF EYE FATIGUE ARE RELATED TO THE WAY WE USE SMART DEVICES, NOT THE BLUE LIGHT THEY EMIT," AAO SAID. "
3.黃斑部病變要怎麼保養?
早期黃斑部病變患者需要特別注意飲食健康,儘量攝取護眼營養素,也要保持血壓、膽固醇及血糖在正常範圍內,才能有效維護眼睛健康。外出時佩戴防紫外線的太陽眼鏡,可以避免紫外線對黃斑的傷害。
4. 如何改善黃斑病變?
除了日常需攝取足夠的營養素去幫助減緩乾性黃斑病變的進展,也可以注射抗血管內皮生長因子藥物以減少新生血管的生長和滲漏。更多改善黃斑病變的方法可以向我們的眼科醫生進行諮詢,醫生會根據你的個人狀況給出適合的治療方案。
5. 黃斑部病變會失明嗎?
有機會導完全失明,黃斑部的的異常新生血管或滲出物可能會對感光細胞造成影響,導致失明。因此,在確診黃斑部病變後需要時刻監察病情是否加重,並尋找醫生進行治療。
6. 怎樣預防黃斑病變?
預防黃斑病變需要定期進行眼科檢查,尤其是有家族病史或年齡超過65歲的人,以便早期發現和治療。保持健康的生活方式,包括均衡飲食、定期運動和戒煙,對預防黃斑病變也很重要。
